Are There Dietary Changes That Can Help Manage Ulcerative Colitis?

Living with Ulcerative Colitis (UC) can be challenging. Painful flare-ups disrupt our daily lives. According to many doctors, there is no Ulcerative Colitis diet plan. But research and experiences show that smart dietary changes can manage symptoms, reduce inflammation, and support gut healing.
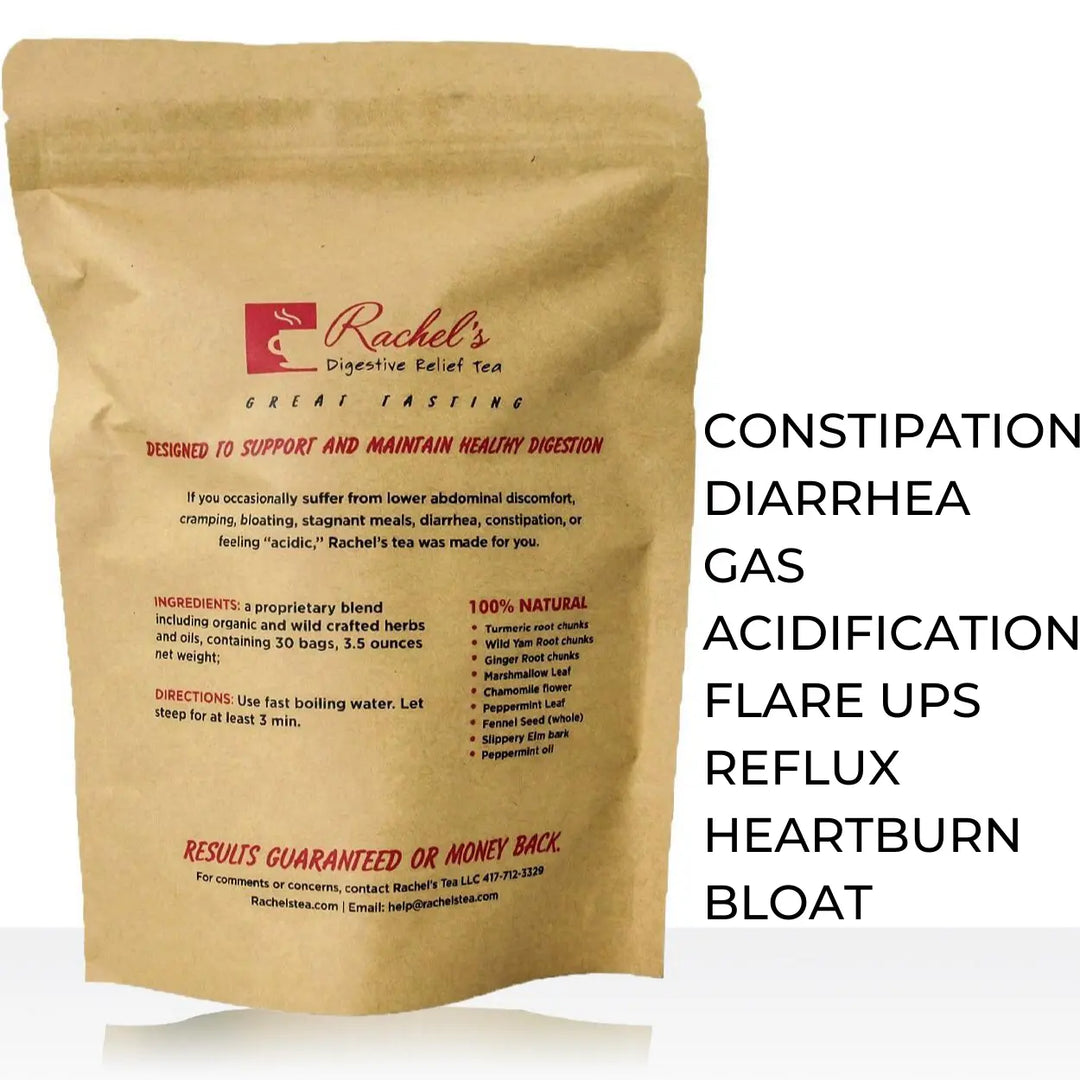
At Pain Free Foods and Rachel’s Tea, we’ve seen how proper nutrition for ulcerative colitis and mindful eating can transform digestive health. Today, we will find practical diet tips, foods to avoid, and lifestyle recommendations for ulcerative colitis.
Understanding Ulcerative Colitis and Digestive Health
Ulcerative Colitis is a chronic inflammatory bowel disease (IBD). It causes inflammation and ulcers in the lining of the large intestine (colon). This inflammation can lead to
- Abdominal pain
- Diarrhea
- Fatigue
- Weight loss
The goal of managing UC is not just to stop flare-ups through the right foods and hydration. Its main goal is
- Support gut healing
- Rebuild the intestinal lining
- Balance gut microbiota
- manage their side effects
Calorie and Nutrient Balance

Unless you are struggling with weight loss due to inflammation and poor appetite. You do not increase your calorie intake. You need to focus on nutrient-dense foods. This will support your gut recovery. These foods should be rich in
- Protein
- Vitamins
- Minerals
If you experience rapid weight loss. Consult a registered dietitian or gastroenterologist. They will create a personalized ulcerative colitis nutrition plan for you.
Fluids and Electrolytes for Gut Health
Hydration is also very important for inflammatory bowel disease. Try to drink at least half your body weight in ounces of water daily. Like, if you weigh 120 pounds, drink about 60 ounces of water per day.
During and after flare-ups, increase your liquid intake with exercise. You can take it in the form of
- Water
- Herbal teas
- Electrolyte-rich drinks
Some drinks worsen dehydration and trigger acid reflux and bloating. Avoid
- caffeinated sodas
- energy drinks
- alcohol
Identifying Problem Foods and Triggers
A single ulcerative colitis diet that works for everyone. Certain types of food can help or hurt us. We should identify our trigger foods. Keep a food and symptom journal to yourself. It will help to track how different meals affect you.
Common triggers include:
-
Fried and greasy foods
-
Spicy dishes
-
High-fat meats
-
Caffeine and carbonated drinks
-
Alcohol and processed sugar
At Pain Free Foods, we have developed a UC-friendly diet plan. It helps people avoid “catalyst food combinations” that worsen inflammation. This plan has helped thousands of people. People have experienced relief by following this method alongside Rachel’s Tea for digestion.
Diet Recommendations During a Flare-Up

During a UC flare-up, you should keep a diet rich in nutrients. At that time, the main goal is to rest your digestive system. You should eat:
-
Cooked vegetables
-
Proteins (chicken, fish, eggs)
-
White rice and oatmeal
-
Omega-3–rich foods like salmon and flaxseed oil
Avoid:
-
Raw fruits and vegetables
-
Whole grains
-
Caffeine and alcohol
-
Dairy (if sensitive)
-
Sugary foods and fruit juices
You can go for a 3-day liquid diet. It includes broths, rehydration drinks and herbal teas. They calm inflammation and support gut repair. To know more about it read Why would I do a liquid diet?
Diet Recommendations After a Flare-Up
Once your UC symptoms improve and you’re in remission. Gradually reintroduce high-fiber and probiotic-rich foods into your diet.
Include:
-
Yogurt, kefir, or probiotics for gut bacteria balance
-
Fruits and vegetables (in small amounts, cooked or blended)
-
Whole grains like quinoa and brown rice
-
Calcium-rich foods such as tofu or fortified plant milk
Eat 4–6 small meals per day. Chew it slowly, and stay hydrated. Switch what you drink with water, broth, tomato juice, and rehydration solutions. Avoid beverages, sip them slowly, which prevents gas and bloating.
Treatments, Nutrition, and Gut Support
While diet alone cannot cure ulcerative colitis. Combining good nutritional choices with medical care can improve your quality of life.
Some UC medications can deplete nutrients like iron, calcium, and vitamin D. So, replenishing these through diet or supplements is necessary. Before making any drastic changes, get in touch with your healthcare provider to ensure you’re making the best choices for your condition.
After years of research at Pain Free Foods, we’ve learned through personal experience that excess acid production and poor food combinations may be major contributors to UC flare-ups. By removing trigger foods, we can support the gut with natural herbs. Inflammation can be reduced or even eliminated.
Related articles:
- Supplements, diet, or a combination of both for digestive relief
- Living With Inflammatory Bowel Disease: What Helped Me Feel Better
Rachel’s Tea: Natural Support for Digestive Disorders
We believe that the inflammation that leads to UC flare-ups is completely preventable and reversible. When we stop eating in a way that causes inflammation in the first place, it will “eliminate symptoms.” If you would like to start your journey to better digestive health, please join us. We have helped hundreds of thousands just like you who are suffering and in pain.
Along with our Pain Free Foods diet plan, our health researchers have formulated a best-selling tea called Rachel’s Tea to quickly get relief. We also have support groups, lots of recipes, and much more! Let us get your quality of life back, starting today! This anti-inflammatory tea supports gut lining repair, reduces bloating, and provides symptom relief for people with ulcerative colitis, IBS, and acid reflux.